Uncooperative patients, unnatural and uncomfortable examination positions and, last but not least, the duration of an examination are common challenges during MRI examinations. Enormous time pressure due to the large number of examinations, frequent preparations of the coils and required setups as well as difficult communication with the patient can make efficient and coordinated work very difficult.
Positioning techniques must be adapted to technical possibilities, the indication itself as well as patient’s needs. Very often, there are several positioning options to achieve the desired result, and the patient's comfort must never be neglected....
For employees who are new to the MRI environment, this variety of options can be overwhelming and lead to uncertainty. However, most of the variations can be easily mastered with a little practice and by complying with certain "basic rules".
When positioning a patient, there are some basic rules that should be followed in every MRI examination - we will go into some of them during this blog. The following Do’s & Don’ts of patient positioning should serve here as an orientation to be able to work safely without neglecting the essentials and the safety of the patient and staff. Good patient positioning is the requirement for good images - which are essential for a diagnosis.
THE DON'TS OF PATIENT POSITIONING IN MRI
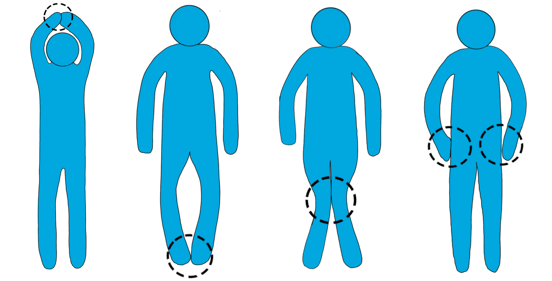
DON'TS: CONDUCTOR LOOPS - WHEN HANDS OR LOWER LEGS TOUCH.
Patient safety is of top priority. Using a standardized “Safety Questionnaire" as well as some “patient positioning safety standards” help in the daily routine. However, especially in the case of standardized positioning, particularly during quick exams with healthy patients, this routinized work can lead to insufficiency, or no attention being paid to important little things. One of these little things is the folding of the hands or crossing of the legs, in case patients are undressed.
Moderate, small burns are reported frequently during or after an MRI. Sometimes, these result from skin contact with the RF coil or the inner wall of the scanner. A more frequent occurrence has been reported with skin-to-skin contact. These areas heated, which again can lead to burns. This risk is particularly prevalent in corpulent patients, on the elbows and upper arms. In most cases, this is only felt as a slight warming during the examination, but it can develop into a burn afterwards.
WHAT MUST BE PAID ATTENTION TO IN ORDER TO AVOID BURNS DURING AN MRI?
- The hands, lower legs or thighs should not touch. If necessary, place a cloth or thin pillow between the legs and/or the armpits.
- Accompanying persons, for example during examinations of children, should not touch the patient's skin directly.
- Even touching the gantry with bare skin during the examination, can cause burns
- The coils should not have direct skin contact; again, some paper sheets or the foam spacers provided by most manufacturers should be used.
- Electrical wires, as in ECG exams, should never be put directly on the skin.
- Patients with unknown textiles or implants on/in the body whose MRI compatibility cannot be verified should not be placed in the MRI.
- Patients should not sweat or have wet hair.
- Wet underwear, diapers, and bandages should be removed.

DON'TS: NEGLECTING ISOCENTRIC POSITIONING
Isocentric positioning is vital for good image quality. If the region of interest, the joint or organ, lies outside the isocenter of the gantry or coil, magnetic field inhomogeneities will occur which will have a negative impact on image quality. When positioning the patient, one sets the foundation for an isocentric position and thus for optimum image quality.
HERE ARE SOME EXAMPLES OF WHAT YOU SHOULD PAY ATTENTION TO IN ORDER TO ENSURE AN ISOCENTRIC POSITION:
.png?width=436&name=MRT_PEarlFit_Wedge-2%20(1).png)
-
For an MRI of the wrist or elbow in supine position, with a flexible surface coil, the patient should slide to the opposite side as far as. Both, joint and coil are thus placed further into the center of the table, consequently also in the isocenter, since the magnetic field at the edge of the table is often not optimal for good image quality.
-
The joint and/or organ in question should be placed in the center of the coil. Decentered positioning is particularly noticeable in the abdomen at the edge of the liver. In addition to the artifacts caused by the heart and lungs, it is not uncommon for artifacts to occur here because the coil ends just above the liver and the isocenter is at the level of the belly button.
These were some important aspects to be avoided in the context of patient positioning in MRI. The following section will cover some “basic rules” that need to be followed.
THE DO'S OF PATIENT POSITIONING IN MRI
DO'S: ACTIVE AND REASSURING COMMUNICATION WITH THE PATIENT DURING PREPARATION AND POSITIONING
For a patient lying motionless 10-60 minutes in the narrow MRI gantry, often in a rather unnatural position, can feel like an eternity. It doesn't even have to be a particularly difficult position, such as for breast, wrist, or elbow scans, which are usually positioned in prone position. Even in supine position, patients complain about pain, for example in the lumbar spine or in the legs. Pressure points in the elbow area also occur repeatedly, as they rest directly on the MRI tabletop.
Even the slightest pressure can lead to unbearable pain during the examination. During an MRI scan, patients have "time" and they can think of nothing else anymore. This repeatedly leads to interruptions or terminations of the MRI, which has a considerable effect on the overall.
HOW CAN ACTIVE AND REASSURING COMMUNICATION GREATLY REDUCE EXAMINATION INTERRUPTIONS?
- Before positioning the patient: It is important to ask the patient where and in which positions pain occurs. This gives ideas of possible complications and allows to adapt the patient positioning to prevent pain.
- During the positioning: Actively solicit feedback from the patient whenever possible. Concerns and pain of the patient should be addressed in the best possible way.
- During the examination, occasional interactions with the patients, e.g. about the remaining time, can lead to better "cooperation" of the patient.
DO'S: PRACTICE, PRACTICE, PRACTICE - FOR EFFICIENT POSITIONING PROCESSES.

Not every patient is the same. Increasing age, weight, and illnesses are more and more leading to MRI setups that are truly challenging. "Special cases" are becoming routine and difficult examinations are becoming commonplace. This requires quick adaptability, proactivity and creativity in the respective situation, as otherwise enormous delays in the examination program can be the result.
In order to be prepared for these situations, it is advisable to take on the role of the patient and try out different approaches and tools together as a team. These "hands-on sessions" often lead to an exciting exchange of experiences within the department and allow new “standard” approaches to be developed.
HOW TO PRACTICE PATIENT POSITIONING IN MRI TO ENSURE AN EFFICIENT POSITIONING PROCESS?
- Take the role of a patient and place yourself in the MRI to see how comfortable or uncomfortable it is to lie in the MRI with available positioning aids.
- Plan and run sequences for "practice exams" to see if reasoning was correct and everything is working.
- Involve radiologists in training so the doctor can see what is possible and what is not.
Particularly because of the tighter examination cycles at the MRI and the time pressure that goes with them, the "routine examinations" should also be practiced again and again as a team. In doing so, it is possible to select appropriate positioning aids in the team, to structure the MRI room together and to standardize work processes. This makes it possible to significantly reduce preparation time as well as positioning efforts and to ensure adequate, i.e. comfortable and stable, positioning on a recurring basis. In addition, the number of interruptions and repeated sequences, which in turn are among the main reasons for delays, can be sustainably reduced. Practicing and optimizing positioning procedures is therefore worthwhile in many respects.
In addition to these basic principles, there are numerous other aspects that must be considered in the respective investigations. These are only some of the possibilities. They form the basis of patient positioning at the MRI and are a basic prerequisite for successful examination procedures and results.
Credits to: Dorina Petersen for providing this content
ABOUT PEARL TECHNOLOGY
Pearl Technology AG, based in Schlieren, offers innovative solutions for the placement, positioning and immobilization of patients in radiology and radiotherapy. The products are manufactured in Switzerland according to ISO norm 13485 and are characterized by simple handling, high patient comfort and excellent hygiene which guarantees smooth and safe examination processes.