Magnetic Resonance Imaging (MRI) remains a cornerstone in diagnostics, yet certain examinations pose unique positioning challenges, notably in Cardiac MRI, Elbow, Wrist, Hand, and imaging on kyphotic patients, just to mention some of the most challenging ones. Also, certain patient cohorts (i.e., paediatric patients, and those with dementia or neurodiversity), offer an extra layer of complexity when properly positioning a patient for their MRI examination. This article explores the complexities of patient positioning in these specific MRI examinations and offers tailored strategies and approaches for a better diagnosis outcome, by aiming to optimize image quality while prioritizing patient comfort and cooperation.
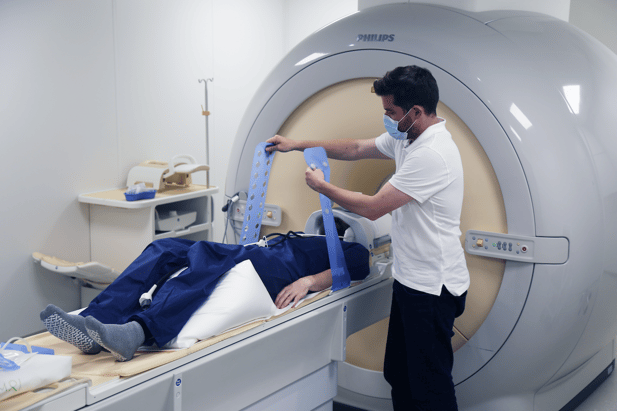
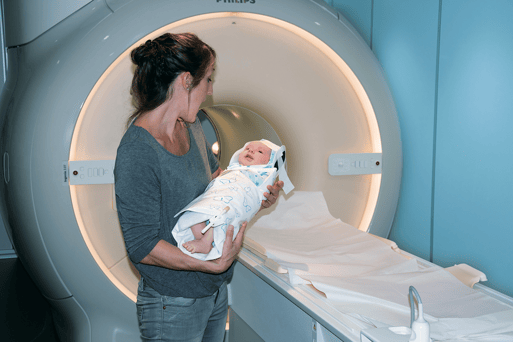
We are all aware of the importance of no movement during MRI examinations in order to obtain optimal diagnostic images. However, when examining certain anatomical structures and patient cohorts as the ones mentioned above, great image quality will be intrinsically connected to optimal patient positioning. Some of these scans are long, and demand a lot from the patients, from constant breath holds in the CMRI case, to laying in the “superman position” for long periods of time as for the Elbow, Wrist and hand scans (if following the positioning golden standard). Adding to this, we have the paediatric cohort that adds a whole other level of challenges as our patients are usually not familiar with hospital grounds and very prone to fear any new environments. This gets even worse if we stop and think about the MRI scanner and room. Placing a sick kid, alone or with a parent in a strange, noisy and daunting environment, will never play in our favour if not planned ahead.
Similar to the paediatric cohort, we have also neurodiverse patients and dementia. In all these cohorts, a lot of intricate factors will play a role on obtaining a great diagnostically valuable MRI image. For the purposes of this article, I will focus solely on positioning.
Challenges in Specific MRI Exams
Cardiac MRI - In this complex examination, a multitude of factors will contribute for a good diagnostic image. Positioning will take a big role as the patient will be lying flat on their back for quite some time while performing several breathing exercises. During a CMRI, precise synchronization with the heartbeat complicates patient positioning, requiring careful coordination for optimal image acquisition by means of ECG. With the amount of cabling and coils around and on the patient, it is paramount that the patient feels comfortable and free of pressure points on the back, shoulders, head and legs in order to better cooperate with the instructions and remain as still as possible. CMRI is a scary scan for any patient, and the need to multitask while nervous, makes it even more challenging for anyone laying on a cold dark tunnel, blasting weird noises every other second.
Upper Extremity Imaging (Elbow, Wrist, Hand) - Capturing detailed views while accommodating varied arm positions, poses specific challenges, impacting image quality and diagnostic accuracy. We are all familiar with the “superman position” which allows us to have the upper extremities in a proper anatomical position (patient laying prone on the table with arms stretched up, hand facing down) while scanning our patients without the risk of having our images flipped and incorrect laterality readings on the reports. This positioning comes with a lot of challenges for all cohorts of patients as laying on the belly for long periods of time, without being able to move and while having a stiff shoulder and a massive speaker shouting at your ears becomes a feat achievable by only a few. In some occasions we do scan patients in supine position (head or feet first), with the arms by their side which is not the golden standard for a multitude of reasons, but it is the only solution when having claustrophobic patients for example, or even when dealing with elderly patients that can’t raise their arms.
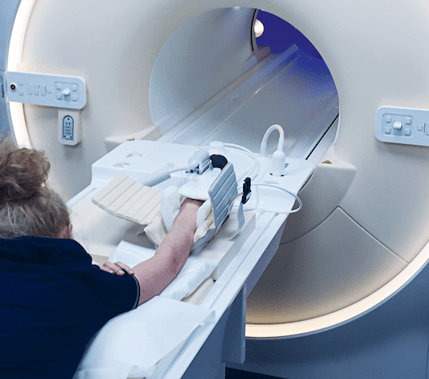
Kyphotic Patients – This cohort of patients, suffer from a condition that originates a curving of the spine that causes a bowing or rounding of the back. This leads to a hunchback or slouching posture. Imaging the head and/or cervical spine in patients with kyphosis demands unique positioning adjustments to attain clear images despite spinal curvature. Usually, these patients struggle to lay flat on the head coil, and this poses a great issue for the radiographers. Head coils are almost in every scanner/manufacturer an inflexible, unbendable, unmovable cage. This feature makes it difficult for any kyphotic patient to undergo a MRI scan of the Brain, C. Spine or any other anatomical structure that involves the patient lying flat on the table. While in other anatomical structures, positioning is important to make sure the patient is comfortable and does not move, in this situation, patient positioning is THE most important aspect of the whole scan as if done appropriately it will make the scan possible or not.
Challenges in Specific MRI cohorts
Paediatric Patients - Cooperation difficulties and the need for specialized approaches to alleviate anxiety and ensure stillness present distinct challenges in this cohort of patients. Humans are born with only two innate types of fear: fear of falling and fear of noise. MRIs are all about noise, hence the challenge to deal with paediatric patients, mainly when under 4 years old. On top of the fear of the noise, there is the reduced attention span issue and of course the lack of understanding of what is going on around them. All these are challenges that will hinder a great MRI diagnostic image.
Patients with Dementia – This cohort of patients requires a whole section of its own. However, I will briefly touch this topic by addressing the main challenges we radiographers face when scanning these patients. Patients with dementia, often have troubles with their memories, mechanical functions of their bodies, and most importantly issues of comprehension that affects their behavioural stance. More often than not, these patients are accompanied by their carers or close relatives, and need constant assurance before, during and after the scan. Patient positioning plays an important role, but several other aspects must be in place in order to achieve good diagnostic outcomes.
Patients with Neurodiversity - Communication barriers and heightened sensitivity to the MRI environment (including lightening, noise, music or lack of it) require tailored strategies to ensure successful imaging. This cohort of patients will pose some specific challenges to the clinical teams as these patients often need a set of adaptations to be made not only to the MRI environment itself as well as to the workflow due to their sensory sensitivities and communication preferences.
Strategies to Overcome Positioning Challenges
Customized Positioning Tools – There is an ocean of dedicated tools that help properly position a patient and overcome all the challenges mentioned above. Utilize tailored devices like flexible coils (i.e., new GE AIR technology) or pads/adjuncts designed for specific scans (e.g., dedicated cardiac, elbow and wrist coils) to aid in maintaining desired positions. Companies like Pearl technology AG also offer a huge selection of dedicated positioning adjuncts that help overcome positioning challenges in specific anatomical parts and specific patient cohorts. Another good example of this adjuncts is the Khypholift tool developed to deal specifically with Kyphotic patients undertaking MRI scans.
Adaptive Protocols - Employ sequences that accommodate variations in heart rate for Cardiac MRI, and shorter acquisition times for paediatric or challenging patients to minimize motion artifacts. Tailored protocols to the patient in front of you are key for a successful examination. Simply running a T2 BLADE/Propeller/MultiVane/JET/RADAR on a brain scan for example, can go a long way between having no diagnostic pictures and having at least one good sequence.
Patient-Centric Care - Prioritize patient comfort and cooperation through clear, effective and assertive communication, distraction techniques like entertainment tools, and music. These can be especially crucial for paediatric, dementia, or neurodiverse patients.
Specialized Training - Equip staff with comprehensive training on handling specific challenges posed by kyphotic patients or those with neurological conditions, ensuring proficiency in adapting techniques. Patients with dementia and or neurodiversity will require different approaches and it is imperative that the clinical teams dealing directly and indirectly with them have the proper training in place and the tools available to approach these patient needs. Even if most NHS hospitals and private healthcare companies have a Dementia champion on their workforce, the overall lack of knowledge and training related to dementia and neurodiversity, allied to the lack of formal guidelines, and lack of standardisation of protocols creates a challenging environment for radiographers and ancillary staff to deliver the quality of service we should all strive for.
Collaborative Approach - Foster teamwork among radiologists, radiographers, and ancillary staff to address unique challenges collectively, streamlining workflows and troubleshooting effectively. Once again, effective, clear and assertive communication is essential when explaining the examination and importance of proper positioning to the patient and their chaperones in order to achieve excellent diagnostic images.
Creativity and empathy – In my humble point of view, these are the most important techniques to overcome any, and I repeat it, ANY challenge we radiographers face on our day- to-day activities. Being creative can go a long way when positioning a patient, by using alternative coils or pads. Maybe scanning a hand in a head coil or an elbow in a shoulder coil can make a huge difference on how a patient will behave during the scan. Understanding that patients are scared not only about the scanner but mainly about the results, and finding a way to resonate with them will definitely make them more cooperative and at ease.

Takeaways
In conclusion, addressing patient positioning challenges in specific MRI exams and patient cohorts demands a tailored approach encompassing specialized positioning tools, adaptive protocols, patient-centric care, and a cohesive, trained team. By implementing these strategies, healthcare providers can navigate these complexities, optimizing image quality and patient experience across diverse MRI examinations and patient populations.